Valuable Information and Advice About Our Gastrointestinal Procedures
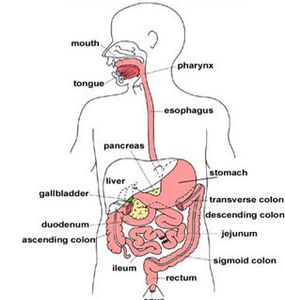
An endoscope is a medical device containing a flexible tube, a light, and a camera. It is used by expert physicians to look inside the digestive tract. Endoscopy allows the physician to examine the lining of the gastrointestinal (GI) tract, which includes the esophagus, stomach, duodenum, colon, and rectum. The physician controls the movement of the flexible tube using the endoscopy handle.
Colonoscopy
Normal Colon and Malignant Polyp
Normal Colon and Malignant Polyp
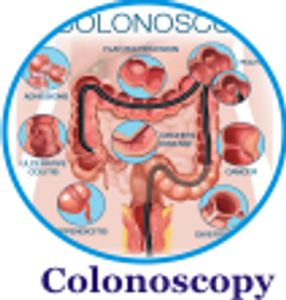
Colonoscopy is a procedure that enables a physician (usually a gastroenterologist) to directly image and examine the entire colon. It is effective in the diagnosis and/or evaluation of various GI disorders (e.g. colon polyps, colon cancer, diverticulosis, inflammatory bowel disease, bleeding, change in bowel habits, abdominal pain, obstruction, and abnormal X-rays or CT scans) as well as in providing therapy (for example, removal of polyps or control of bleeding). It is also used for screening for colon cancer. A key advantage of this technique is that it allows both imaging of abnormal findings and also therapy or removal of these lesions during the same examination. This procedure is particularly helpful for identification and removal of precancerous polyps.
Normal Colon and Malignant Polyp
Normal Colon and Malignant Polyp
Normal Colon and Malignant Polyp
A gastroenterologist is a specialist in gastrointestinal diseases and has received special training in colonoscopy. Gastroenterologists perform more colonoscopies by far than any other specialty. Non-gastroenterologists are five times more likely to miss colorectal cancer during colonoscopy than Gastroenterologists.
Proper training in colonoscopy is necessary not only to increase the chance that the procedure can be completed and any necessary treatments applied but also to be sure that abnormal results can be properly interpreted.
The American Society for Gastrointestinal Endoscopy recommends that persons performing colonoscopy complete a fellowship program in gastroenterology or receive training in colonoscopy during a surgical residency.
Experienced colonoscopists reach the very beginning of the large intestine (the cecum) in more than 90% of cases and in more than 95% of patients who are undergoing screening. Screening is the process of checking people who have no symptoms of colon polyps and cancer.

EGD
The term “endoscopy” refers to a special technique for looking inside a part of the body. “Upper GI” is the portion of the gastrointestinal tract that includes the esophagus, the stomach, and the duodenum which is the beginning of the small intestine. The esophagus carries food from the mouth for digestion in the stomach and small intestine. EGD is a procedure performed by a gastroenterologist, a well-trained specialist who uses the endoscope to diagnose and, in some cases, treat problems of the upper digestive system.
The endoscope is a long, thin, flexible tube with a tiny video camera and light on the end. By adjusting the various controls on the endoscope, the gastroenterologist can safely guide the instrument to carefully examine the inside lining of the upper digestive system. The high-quality picture from the endoscope is shown on a TV monitor; it gives a clear, detailed view. In many cases, EGD is a more precise examination than X-ray studies. EGD can be helpful in the evaluation or diagnosis of various problems, including difficult or painful swallowing, abdominal pain, bleeding ulcers, and tumors. Tiny instruments can be passed through an opening in the endoscope to obtain tissue samples, coagulate (stop) bleeding sites, dilate or stretch a narrowed area, or perform other treatments.
Before the Procedure
Before the Procedure
Before the Procedure
Regardless of why upper GI endoscopy has been recommended for you, there are important steps you can take to prepare for and participate in the procedure.
Talk to Your Doctor
Before the Procedure
Before the Procedure
First, be sure to give a complete list of all the medicines you are taking—including any over-the-counter medications and natural supplements—and any allergies to drugs or other substances. Your medical team will also want to know if you have heart, lung, or other medical conditions that may need special attention before, during, or after an EGD. It is important they know if you are taking diabetic medications or anticoagulants (blood thinners) or have bleeding or clotting problems.
Breath Test
Breath Test
Breath Test

Helicobacter Pylori (H Pylori) testing is especially performed in patients suspected of having gastritis, gastric ulcers, and duodenal ulcers. The test measures active H. Pylori infection.
Your gastroenterologist might rely on a Urea Breath Test (UBT) to test for the presence of H. Pylori. "If an infection is present then the bacterium's urease enzyme breaks down urea in the stomach releasing carbon dioxide and ammonia". This test is used for the initial diagnosis and post-treatment monitoring of H Pylori infection in the stomach. The test should only be performed 14 days after stopping acid-reducing medication (proton pump inhibitors) or 28 days after stopping antibiotic treatment. The Breath Tek UBT kit is for administration by a health care professional, as prescribed by a physician.
ERCP
Breath Test
Breath Test
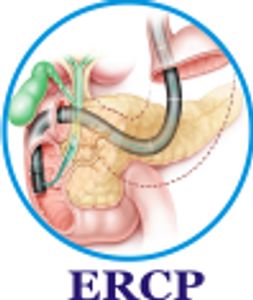
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that uses X-ray to view the patient's bile and pancreatic ducts.
The functions of the common bile duct and the pancreatic duct are to drain the gallbladder, liver, and pancreas. The most common reason why someone would need an ERCP is because of a blockage of one of these ducts.
ERCP Preparation
You will be asked not to eat or drink anything for six to eight hours before the test. Once the scope is inserted through the mouth, esophagus, stomach, and intestine. A small plastic tube (cannula) is passed through the endoscope into the opening of the bile duct through a structure called the papilla, a dye is injected, and X-ray pictures are taken after the injection and displayed on a TV monitor so the endoscopist can examine the bile ducts and pancreatic duct.
If stones are present in the common bile duct, the opening of the papilla can be widened, and the stones are removed. If the X-ray pictures show a narrowing of the bile duct, a stent can be inserted to allow the bile to bypass the blockage and pass into the duodenum.
PillCam
PillCam SB is the most widely used, patient-friendly tool for directly visualizing the small bowel to detect and monitor abnormalities. This procedure is the standard of care for small bowel evaluation, helping healthcare practitioners detect the presence of lesions that may be the source of obscure GI bleeding, iron deficiency anemia, abdominal pain, or diarrhea.
With PillCam SB, physicians can visualize the entire small bowel without putting their patients through a lengthy, uncomfortable procedure or having them undergo sedation. By simply swallowing a vitamin-sized capsule, physicians may detect and monitor lesions, ulcers, tumors, and bleeding within the small bowel.

Capsule Endoscopy Uses
Capsule Endoscopy Uses
Capsule Endoscopy Uses
Capsule endoscopy provides your doctor with images of your digestive system that cannot be captured with conventional X-rays.
Your gastroenterologist will use the images transmitted by the capsule to diagnose and evaluate a variety of conditions, including:
* Gastroesophageal reflux disease (GERD)
* Barrett's Esophagus
* Diarrhea
* Polyps
* Anemia and bleeding
* Bowel function
* Malabsorption
* Abdominal pain
* Tumors and some cancers
* Celiac sprue
* Crohn’s disease
Your gastroenterologist may also use capsule endoscopy to monitor the progress of treatment plans for these conditions. If your doctor detects a serious problem in your esophagus, you may need to undergo a conventional endoscopy to confirm diagnosis and, possibly, to receive treatment
Esophageal Manometry
Capsule Endoscopy Uses
Capsule Endoscopy Uses
Esophageal Manometry is an outpatient test used to identify problems with movement and pressure in the esophagus that may lead to problems like difficulty swallowing. The esophagus is the "food pipe" leading from the mouth to the stomach. Manometry measures the strength and muscle coordination of your esophagus when you swallow.
The esophagus is a muscular tube that connects the throat with the stomach. When food is propelled by a swallow from the mouth into the esophagus, a wave of muscular contraction starts behind the food in the upper esophagus and travels down the entire length of the esophagus (referred to as the body of the esophagus), thus propelling the food in front of the wave through the esophagus and into the stomach. At the upper and lower ends of the esophagus are two short areas of specialized muscle called the upper and lower esophageal sphincters. At rest (that is, when there has been no swallow), the muscle of the sphincters is active and generates pressure that prevents anything from passing through them. As a result, the material within the esophagus cannot back up into the throat, and stomach acid and contents cannot back up into the esophagus. When a swallow occurs, both the sphincters relax for a few seconds to allow food to pass through the esophagus into the stomach.

When is esophageal manometry used?
Esophageal manometry is used primarily in three situations:
• To evaluate the esophagus when there is reflux (regurgitation) of stomach acid and contents back into the esophagus (gastroesophageal reflux disease or GERD)
• To determine the cause of problems with swallowing food (dysphagia)
• When there is chest pain that may be coming from the esophagus
How is esophageal manometry performed?
At the start of the esophageal manometry procedure, one nostril is anesthetized with a numbing lubricant. A flexible plastic tube approximately one-eighth inch in diameter is then passed through the anesthetized nostril, down the back of the throat, and into the esophagus as the patient swallows. Once inside the esophagus, the tube allows the pressures generated by the esophageal muscle to be measured when the muscle is at rest and during swallows. The procedure usually takes 15 to 20 minutes.
Copyright © 2021 Panhandle Gastroenterology - All Rights Reserved.
Powered by GoDaddy